Finding out about Congenital Heart Defect

We knew and understood from the beginning that our parenthood journey is going to be long and winding with bumps along the way but nothing could have prepared us for the news.
We looked forward to the 20 week anatomy ultrasound scan, rested and relaxed after Christmas and New Year's holiday across New Zealand. We were excited to see the baby's growth and chance to take a peak again. The sonographer started taking usual measurements of fetal organs, body parts to check growth and any structural abnormalities and we got to see so much more than 14 week nuchal scan. What a difference 6 weeks makes in the baby's life. The sonographer kept going back to the heart and spent a lot of time trying to get images needed and we started asking questions. The sonographer told us that the arteries did not look like they crossed-over and it could be a problem with angle but would talk to another sonographer and make a referral to fetal medicine. Waiting back at reception area for a few minutes, the sonographer came back to tell us that there might be a congenital heart defect and would be in touch with our obstetrician for referral to fetal medicine at Auckland hospital, along with booking a follow up ultrasound scan the next week as they couldn't get clear view of spines.
It was one of the longest 7 days we've ever experienced between the 20 week scan, follow up scan, and the fetal medicine appointment. We hoped the follow up scans would be clear and we'd be told everything was as normal. But we couldn't help researching what it could be and found 3 most likely conditions and dived deeper into researching them. Our emotions were going all over the place the whole weekend. It didn't help we did not have confirmed appointment date/time for fetal medicine going into the weekend. We just hoped that the follow up scan would confirm arteries developed as expected and we wouldn't need fetal medicine referral anymore. We felt helpless at this point, as intended parents we are not the patient, patient's family, nor parents and cannot directly receive copies of information or push for updates from healthcare providers ourselves.
In the morning of the follow up scan, 6 days after 20 week scan, Wendy called to say we have the fetal medicine appointment booked for the next day. At last, the wait was coming to an end. At the follow up ultrasound with a senor sonographer, the baby's growth and spine was great. However, in a moment this would all change and learned everything was not great. The sonographer confirmed that fetal echocardiogram is required and we knew that the baby had congenital heart defects. This narrowed down our research down to 2 potential conditions. What was going to happen with pregnancy? What was quality of life going to be like for the baby? How common or rare are the conditions? We had 100 more questions than before.
The next day at the maternal fetal medicine clinic at Auckland hospital we had the same sonographer from the day before. Strangely, this made it a little easier as we did not have to explain again why there are 3 people at the appointment, that we are the parents, and Wendy is the surrogate for the baby. It seemed like no time and eternity passed with all the images, and videos being taken through echocardiogram of tiny heart of our baby. We went back out to waiting area whilst cardiologist review the images and videos. What felt like only a second, we were in a consultation room with a cardiologist, an obstetrician, a Maternal Fetal Medicine midwife, and a paediatric and congenital cardiac specialist nurse.
We started with an introduction on who are the clinical team, who we are, our surrogacy journey, and family medical history. The moment is etched into our memory forever being told that our baby has congenital heart defects known as Transposition of the Great Arteries (TGA) and Ventricular Septal Defect (VSD). Our minds were racing, emotions running high and we had questions after questions. Luckily there was no other issues identified and that the pregnancy will continue normally and we will continue to see our obstetrician and supplemented with the team at Auckland hospital. Although the baby would require on-going cardiac care throughout life, they are expected to grow, live, learn, and play like any other child.
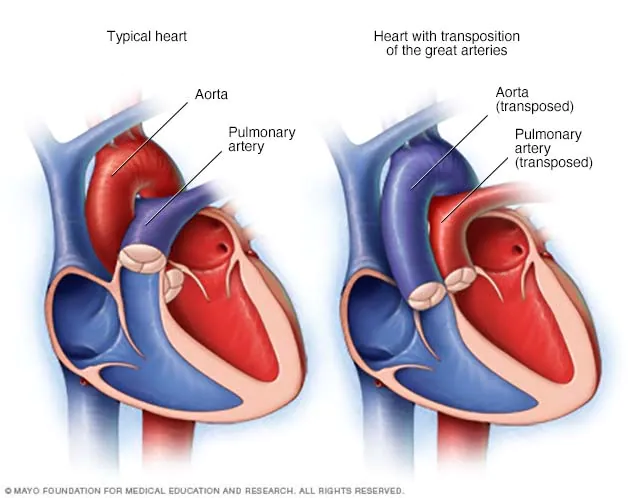
TGA is a condition that affects the two large arteries of the baby's heart that carry blood from heart to the lungs and the rest of the body. Right ventricle pumps blood into pulmonary artery. Then it goes to the lungs where the blood gets oxygen. The blood then returns to the left side of the heart. Then the left ventricle pumps blood to the body through the aorta. With TGA, the pulmonary artery is connected to the left ventricle instead of the right ventricle and the aorta comes from the right ventricle instead of the left. This means oxygen-poor blood pumps back into the body instead of going to the lungs. And the already oxygen rich blood goes back to lungs where it just came from. What this means is that the body and brain does not receive the oxygen and nutrients it needs. At birth, the baby would show low oxygen levels and baby can appear blue due to lack of oxygen in blood.
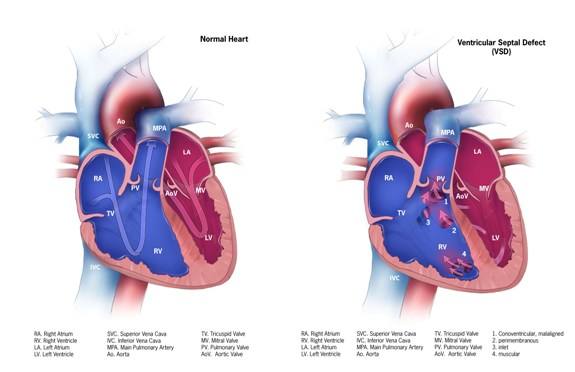
VSD is a condition that has hole between the bottom chambers (ventricles) of the heart and oxygen rich and oxygen poor bloods mix between ventricles. VSD is common with babies with TGA.
The baby will require immediate medical intervention, open heart surgery and likely other surgeries; prostaglandin E1 (medication) will be admistered within minutes of their birth to keep ductus arteriosus open allows blood to flow through the heart until surgery can be done that would otherwise naturally close after birth. The first procedure Balloon Atrial Septostomy (BAS) will happen in first hours of life and Arterial Switch Operation (ASO) in the first few days of life. BAS is a keyhole (cardiac catheter) procedure that enlarges the foramen ovale to allow some blood to mix between the left and right atria. ASO is a major and complex surgery and as the name suggests switches over aorta and pulmonary artery and corrects the coronary arteries to restore normal blood flow through the baby's heart and to the rest of the body. During ASO operation VSD and hole created during BAS would be corrected too. There are about 10-15 babies in New Zealand born (similar to other countries stats of 1 in 3-4000 births) with TGA. There are 3 cardiac surgeons that perform ASO surgery in New Zealand based out of Starship Hospital in Auckland. The babies recovery is likely to be 2-6 weeks after birth, with regular cardic appointments for the rest of their life and potential future interventions surgical or non-surgical as they grow.
The condition means that the birth must happen in Auckland hospital. Luckily our birth plan was already at Auckland hospital and as Wendy lives in Auckland we had one less thing to work through. But all of the post-natal care ideas and plans were scrapped.
We must have spent about 90 minutes in the room with all the questions. As intending parents we have the extra complexity with managing consent for healthcare and to avoid putting stress on Wendy's family as much as possible. Legally we cannot give parental consents ourselves until we have the placement order from Oranga Tamariki, usually given on the day of the birth. We had questions on how it can be planned given likely first operation in the first hours of life.
In an instant our world and our life has changed once more. A very high survival rate, and good long-term prognosis didn't lessen all the overwhelming emotions we were feeling; despair, fear, helplessness, panic, sadness, and hurt. After the appointment we headed back to work for an hour or so and it's a bit of blur. On the way home, we told our immediate family who knew about the appointment on the confirmed diagnosis. It can only be described as a complete meltdown of emotions and ugly cry but we had to start sharing the news. Eventually over the course of a week we had told close friends and families and came up with a communication plan.
Our research to learn more continues but our emotions are often overwhelmed and easily triggered. Who knew how frequently references to heart, family, pregnancy are made in every day life?! We have now found Heart Kids, private Facebook groups for TGA, NZ media stories on other families with the condition; NZ Herald - Kalo story, Stuff - Sohpia story, Stuff - Josiah story, Stuff - Cameron story. We have since accelerated engagement with Oranga Tamariki and our lawyer as these are a few things we can manage and prepare.
We know it will all be OK, we do not know how emotions will come out, but we do know the baby and Wendy are otherwise healthy during pregnancy. We do know we have so much support and love from friends and family and we are absolutely grateful.
Resources
- 2-minutes explainer YouTube video for Transposition of the Great Arteries (TGA) from Children's Healthcare of Atlanta. Provides a good summary of the condition with easy to follow and understand animation.
- Heart Kids NZ is the only national organisation in Aotearoa NZ dedicated to providing free lifelong care and support for children, teens, adults and whānau impacted by childhood heart conditions.
- Media stories for children with Transposition of the Great Arteries (TGA) NZ Herald - Kalo story, Stuff - Sohpia story, Stuff - Josiah story, Stuff - Cameron story

